Build, orchestrate and optimize insurance operations in 1 Platform
Run connected insurance workflows with human-AI collaboration built in.
Four Module Cards
We connect 4 modules into 1 workflow to help you design, manage, and automate insurance with full control.
Experience Flow
Build and launch customer journeys. Your teams design the logic; we help you deploy. The market won't wait. insurers who win adapt their workflows in real time.
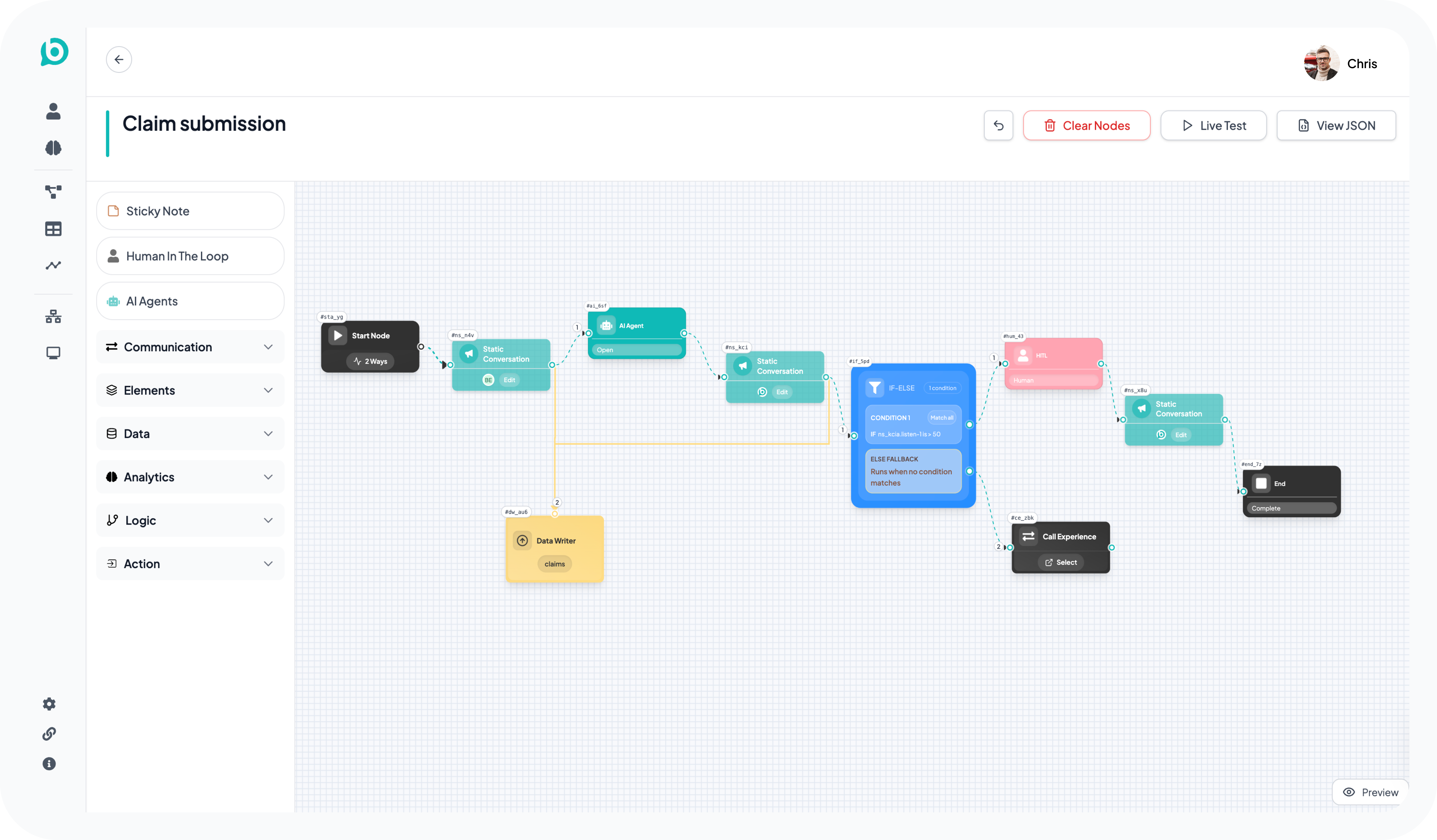
Key Capabilities:
No code builder: Map rules and pathways without developers.
Omnichannel: Deploy to web, mobile, and portals at once.
Personalisation: Use your data to adapt the journey for every user.
Analytics Flow
Turn data into decisions. Your analysts track every journey in real time, using these insights to manage risk and improve performance. Success belongs to insurers who act on what their data is telling them.
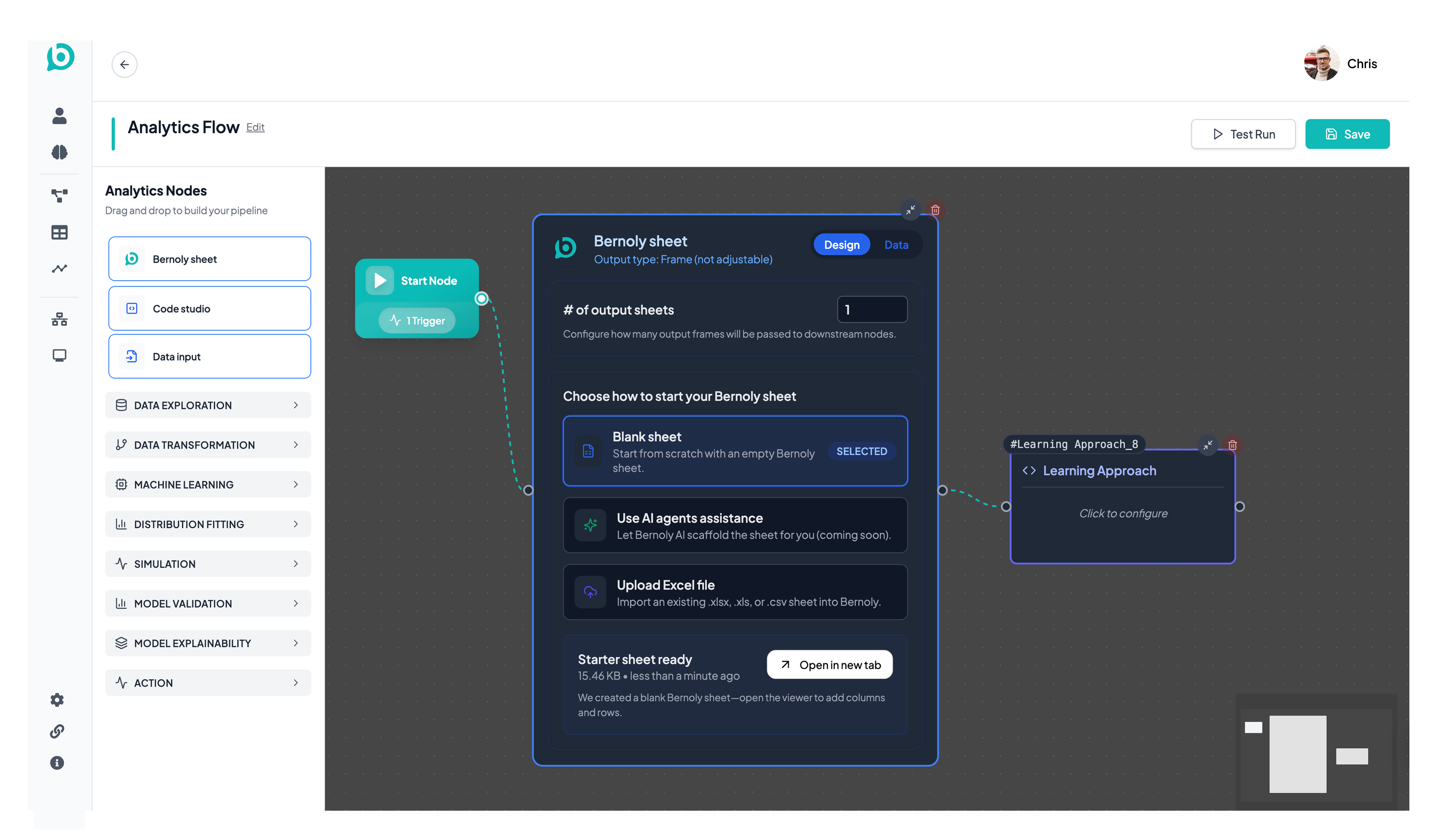
Key Capabilities:
Real time dashboards: Track conversion and find where customers stop.
Anomaly detection: Help your team spot suspicious claims or errors automatically.
Predictive modelling: Forecast demand, lapse rates, and claim frequency.
Human - AI Collaboration
AI agents provide value through end to end workflows, not just models. We help your teams and AI work as one. Your experts set the strategy; our agents handle the process. This is how you scale without losing the judgement that defines your brand.
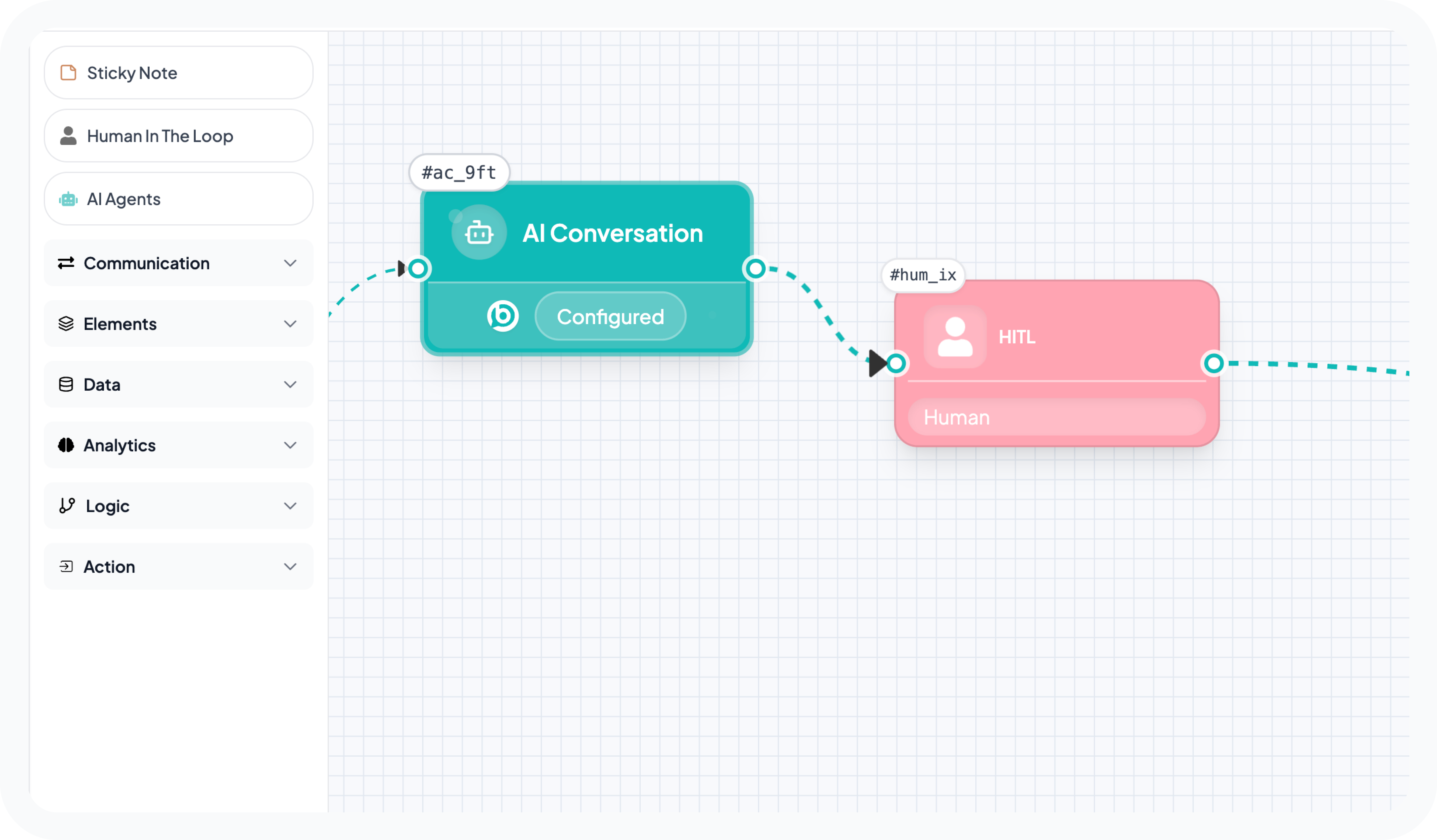
Key Capabilities:
Workflow first AI: Agents that complete tasks across your entire operation.
Seamless handoff: AI flags complex cases for human judgement instantly.
Active learning: Your team’s decisions refine the AI in real time.
Data Atlas
Organised data is the foundation of AI. Data Atlas is your command centre for every asset you hold. We help you see where data lives and how it connects. Your teams win when they work from a single, accurate source of truth.
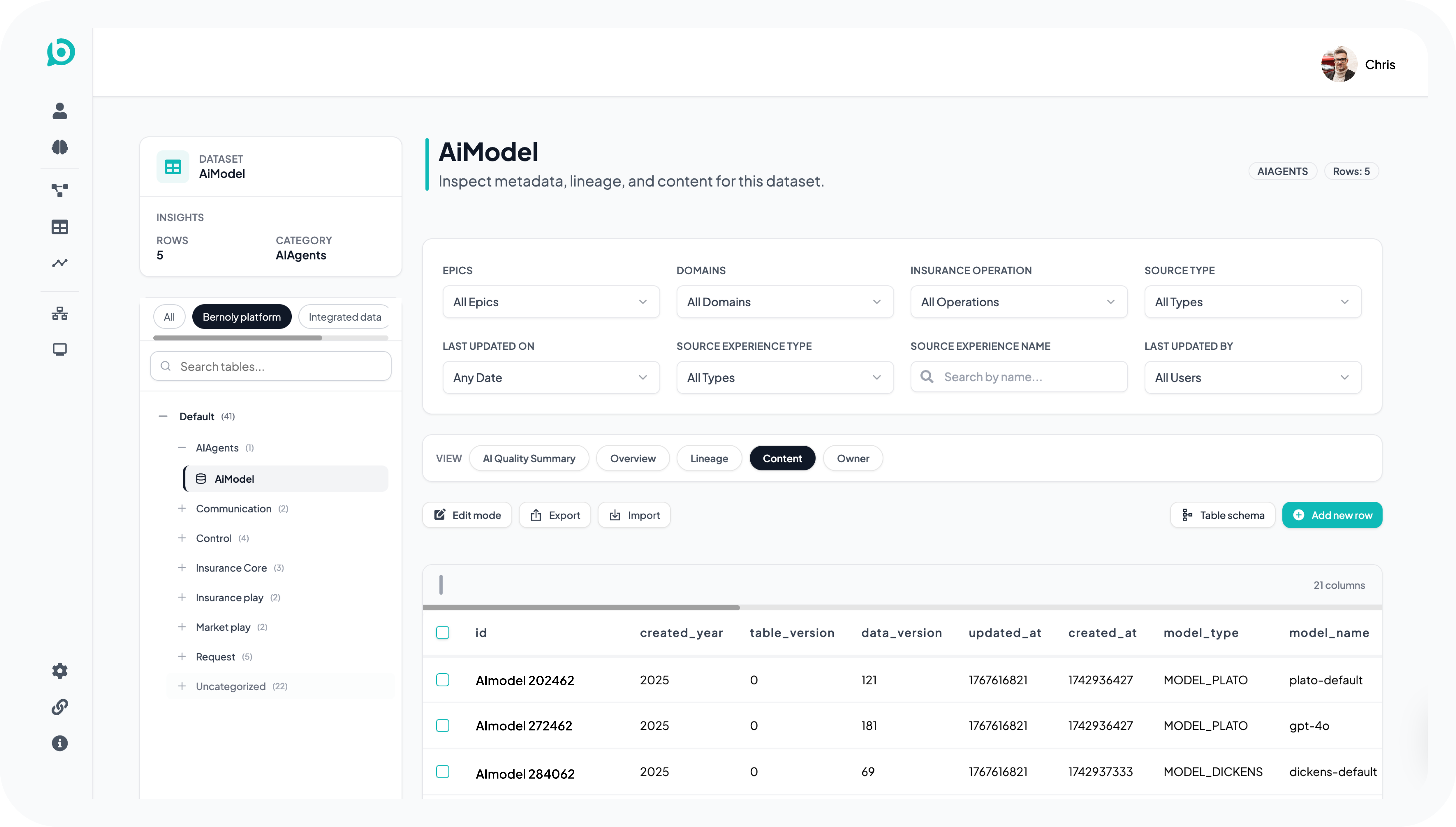
Key Capabilities:
Visual schema: See every table and relationship in one view.
Data governance: Track how data moves to stay compliant.
Live inventory: A clear summary of all your stored assets.





